Emergency Medical Information for Pompe Disease
Be prepared when every second counts.
The AMDA’s Emergency Medical Information resources provide clear, evidence-based guidance for anesthesia and respiratory care — and a free Medical Alert Card that ensures these details are always within reach.
This information is provided for educational purposes only and is not a substitute for professional medical judgment. Health care providers should always refer to their institutional protocols and consult specialists familiar with Pompe disease.
Be Ready to Share the Right Information
Pompe disease presents unique anesthesia and respiratory risks. In emergency or surgical situations, healthcare teams must take special precautions to ensure safe treatment.
These key reminders summarize the most critical points covered in AMDA’s Emergency Medical Information resources and the Medical Alert Card.
Remember: Treat hypoventilation, not just low oxygen.
⚠️ For Emergency Personnel:
Review the Emergency Medical Info overview PDF before administering oxygen or anesthesia.
It summarizes approved medications, ventilation support, and immediate post-anesthesia care guidelines for Pompe disease.
Quick Reference Bullet List
Avoid Suxamethonium (succinylcholine) – may trigger rhabdomyolysis or cardiac arrest.
Never give oxygen alone – always pair with BiPAP or assisted ventilation and monitor CO₂.
Use short-acting, non-depolarizing agents – titrate with Train-of-Four (TOF) monitoring.
Have ventilatory support ready – BiPAP or mechanical ventilation should be available post-procedure.
CPAP ≠ BiPAP – BiPAP supports ventilation; CPAP only prevents airway collapse.
Avoid long-acting sedatives and high-dose opioids – can suppress breathing.
About the AMDA Medical Alert Card
When faced with an emergency, seconds matter, and so does having accurate information in the hands of clinicians
To make that easier, the AMDA developed the Pompe Medical Alert Card, modeled after and created with the kind permission of Breathe with MD, Inc.
This card puts essential anesthesia and respiratory guidance directly in the patient’s wallet, so it’s available the moment emergency personnel or hospital staff need it.
Each card includes a QR code linking to this page, giving health care professionals immediate access to the most current, evidence-based recommendations for Pompe disease care.
The goal is simple: to make sure no patient faces a medical crisis without the right information close at hand.
Free for all Pompe community members — cards can be requested directly through the form below.
Shipping Notice:
At this time, Medical Alert Cards can only be mailed to addresses within the United States.
Outside the U.S.?
We offer a printable version of the card for international Pompe families and individuals.
What’s on the AMDA Medical Alert Card
Carry Critical Information Everywhere You Go
The AMDA Medical Alert Card summarizes vital respiratory and anesthesia information for individuals with Pompe disease. It was modeled after the original Breathe with MD, Inc. card and adapted by AMDA with their permission to reflect Pompe-specific guidance.
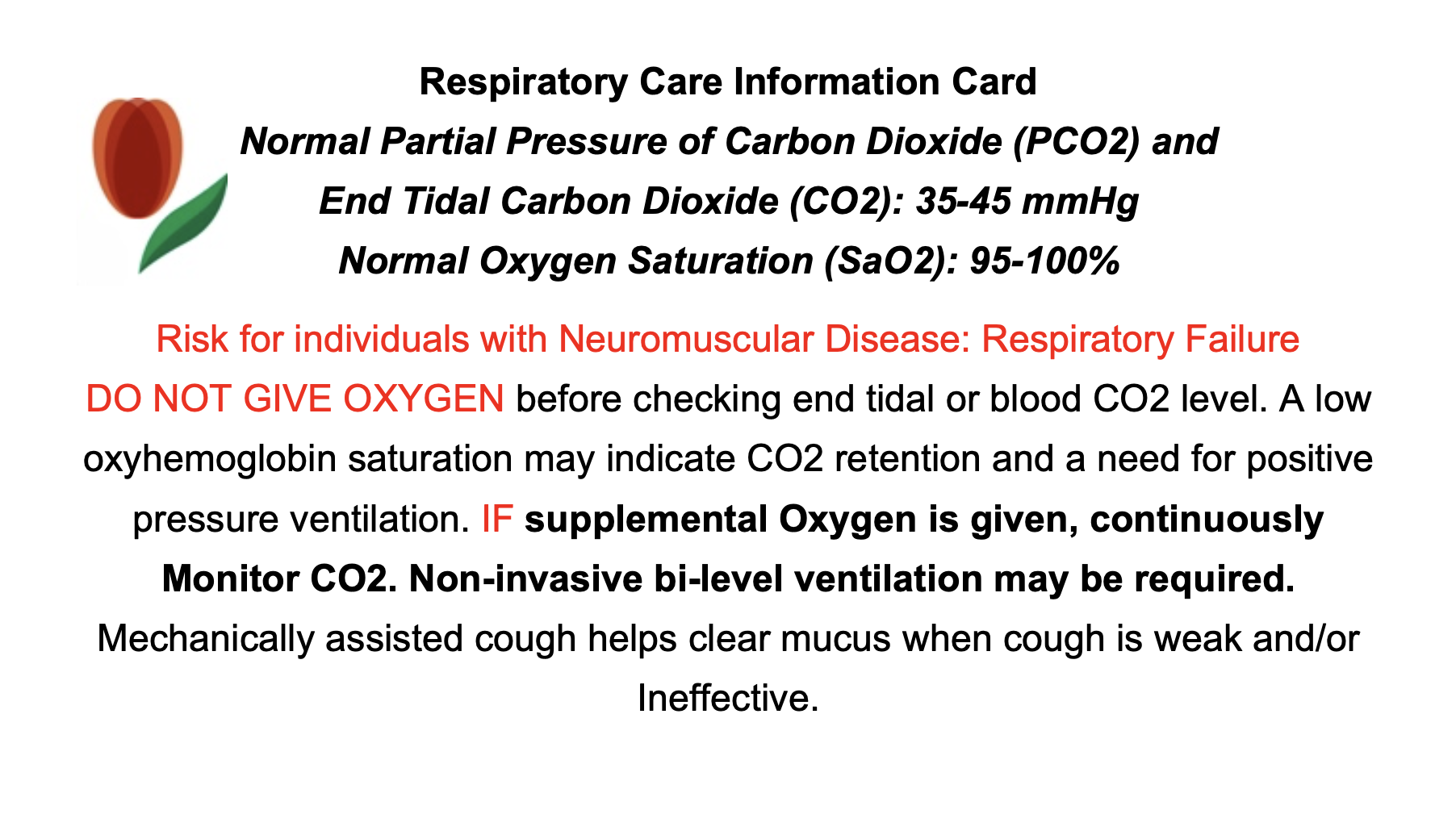
The front of the card lists:
-
Normal blood-gas ranges for CO₂ and O₂
-
A reminder that people with neuromuscular disease are at risk for respiratory failure
-
The directive: “DO NOT GIVE OXYGEN before checking CO₂.”
-
Key ventilation and cough-assist guidance
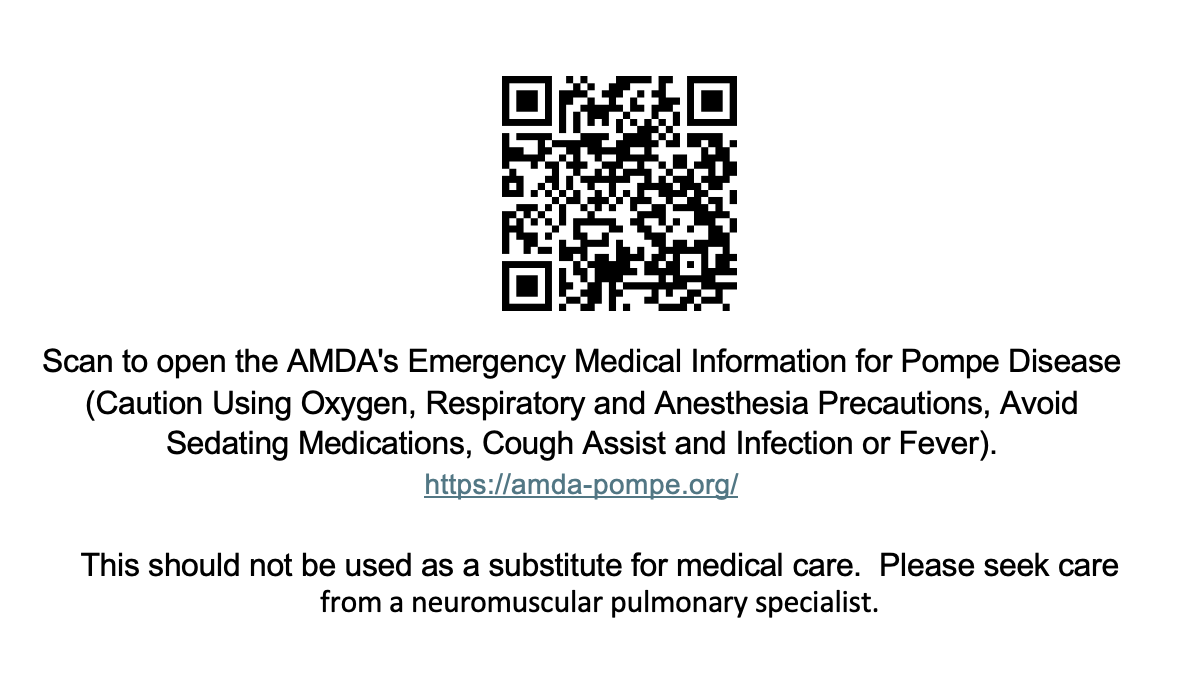
The back includes:
-
A prominent QR code that will link to our Emergency Medical Information & Alert Card page.
-
A brief disclaimer reminding clinicians to seek guidance from neuromuscular respiratory specialists
-
The AMDA logo and tulip tagline for recognition and authenticity
Together, the printed card and this online resource ensure that emergency teams, hospitals, and caregivers have immediate access to accurate, life-saving information.
Request Your Free AMDA Medical Alert Card
The AMDA provides the Pompe Medical Alert Card free of charge to members of the Pompe community.
Each card is printed on durable, wallet-sized stock and includes a scannable QR code linking directly to our Emergency Medical Information & Alert Card page, so the most accurate, up-to-date guidance is always available to healthcare professionals.
Requests are managed by our Patient Advocate, Marsha Zimmerman, who uses the information provided to fulfill card requests and help keep our contact records current.
If you or a family member would like a card mailed to you, please complete the short form below.
Shipping Notice:
At this time, Medical Alert Cards can only be mailed to addresses within the United States.
Outside the U.S.?
We offer a printable version of the card for international Pompe families and individuals.
Medical Alert Card Request Form
Emergency & Respiratory Care Resources
The information printed on the AMDA Medical Alert Card and linked through its QR code is based on these detailed fact sheets.
Each resource below explains a specific aspect of Pompe disease emergency and respiratory care, from safe anesthesia practices to effective ventilation support.
These materials are intended for both patients and healthcare providers, helping ensure that everyone involved in care has the same accurate, up-to-date information.
Emergency Medical Information (Overview)
A quick reference for ER and surgical teams covering oxygen use, anesthesia risks, and safe airway/ventilation steps for Pompe disease. Use this first when time is tight; it links out to all detailed fact sheets.
⚠️ Key Alert: Always assess ventilation as well as oxygenation—do not give oxygen alone if hypoventilation/CO₂ retention is suspected; prioritize BiPAP and monitor CO₂.
Read more about the Emergency Medical overview
Pompe disease weakens respiratory muscles and changes anesthesia risk. In emergencies, check both oxygen and CO₂ (capnography or blood gas). If distress is present, initiate BiPAP promptly and avoid unnecessary intubation. If intubation is required, avoid suxamethonium (succinylcholine) and plan for close post-anesthesia monitoring and possible ventilatory support.
Anesthesia Precautions in Pompe Disease
Pompe patients are highly sensitive to anesthetics and muscle relaxants due to respiratory muscle weakness and potential cardiac involvement. Careful agent choice, TOF monitoring, and postoperative ventilation planning are essential.
⚠️ Key Alert: Avoid suxamethonium (succinylcholine). Use non-depolarizing relaxants in reduced doses with TOF monitoring; plan for postoperative ventilatory support when indicated.
Read more about anesthesia precautions
Assess for hypoventilation even when SpO₂ looks normal; prioritize CO₂ monitoring and non-invasive ventilation when needed. Titrate short-acting agents, use TOF for dosing and reversal, and consider ICU or high-acuity recovery. Coordinate pre-op with pulmonology, cardiology (if relevant), and the neuromuscular team.
Anesthesia Medication Safety List
A quick screen of agents to avoid or use cautiously in Pompe disease. Highlights safer short-acting options and monitoring must-haves to prevent prolonged paralysis or respiratory depression.
⚠️ Key Alert: Avoid suxamethonium. Use caution with volatile anesthetics, high-dose opioids, and long-acting neuromuscular blockers; always use TOF monitoring and confirm full recovery before extubation.
Read more about the anesthesia medication list
Prefer short-acting agents (e.g., propofol/etomidate) with vigilant monitoring. Use non-depolarizing relaxants (e.g., rocuronium/atracurium) with TOF and full reversal. Maintain continuous capnography and pulse oximetry, anticipate postoperative BiPAP/mechanical ventilation, and never give oxygen alone if CO₂ retention is suspected.
Suxamethonium (Succinylcholine) Warning
This depolarizing neuromuscular blocker is contraindicated in Pompe disease due to life-threatening risks. Use safer non-depolarizing alternatives with close monitoring.
⚠️ Key Alert: Do not use suxamethonium due to risk of rhabdomyolysis, hyperkalemia, prolonged paralysis, and respiratory failure; choose short-acting non-depolarizing agents and ensure ventilatory support.
Read more about the suxamethonium warning
Suxamethonium can trigger massive potassium release in myopathic muscle and worsen respiratory compromise. Opt for rocuronium or cisatracurium with TOF guidance, be prepared with reversal strategies, and secure ventilatory support. Document this contraindication prominently in anesthesia plans.
Caution Using Oxygen
In Pompe disease, oxygen can hide underlying hypoventilation and worsen CO₂ retention if given without ventilatory support. Treat hypoventilation first.
⚠️ Key Alert: Never provide oxygen alone; pair with BiPAP/NIV and monitor CO₂ (capnography or ABG). “Treat hypoventilation, not just hypoxemia.”
Read more about using oxygen safely
Because the diaphragm is weak, patients may retain CO₂ even with normal oximetry. Start noninvasive ventilation to improve ventilation and then titrate oxygen if needed, with continuous CO₂ tracking to avoid respiratory acidosis and failure.
Cough Assist (Mechanical Insufflation-Exsufflation)
Helps clear mucus when cough is weak, reducing infections, hospitalizations, and work of breathing; useful daily and during illness.
⚠️ Key Alert: Use individualized pressures and timing under a pulmonologist familiar with neuromuscular disease; integrate with airway clearance plans.
Read more about cough assist therapy
MI-E alternates insufflation and rapid exsufflation to mimic a strong cough, improving airway clearance and gas exchange. Combine with BiPAP, chest physiotherapy/vest therapy, humidification, and suctioning as needed for thick secretions.
CPAP vs. BiPAP in Pompe Disease
CPAP splints the airway (OSA), but does not support ventilation. BiPAP (NIV) provides inspiratory/expiratory pressure support and is preferred when hypoventilation is present.
⚠️ Key Alert: For neuromuscular hypoventilation, choose BiPAP/NIV (often with backup rate) rather than CPAP; initiate based on symptoms/tests of ventilatory failure.
Read more about choosing CPAP vs. BiPAP
Begin NIV when clinical features (orthopnea, morning headaches, daytime sleepiness) and objective data (nocturnal CO₂ rise/desaturation, daytime hypercapnia, low FVC or large supine drop) indicate evolving hypoventilation. BiPAP improves sleep quality, gas exchange, and long-term stability.
More Respiratory Resources
Explore additional reading and clinical recommendations on long-term Pompe respiratory care:
- Publications by Dr. John Bach – foundational research and clinical protocols for noninvasive ventilation and cough-assist therapy in neuromuscular disorders.
- “In the Clinic: Ventilatory Monitoring and Cough Assistance – Dr. Bach’s detailed recommendations for tracking vital capacity, using cough-assist devices, and recognizing early signs of hypoventilation.
- Quest MD Article: “Respiratory Care in Pompe Disease” – an accessible overview of practical respiratory management
Visit our Additional Respiratory Care Resources page to view these materials.